Characteristics
The type of albinism in HPS is a tyrosinase-positive form, which means people with HPS may present with varied amounts of pigmentation. Some people may have very light hair and fair features and be diagnosed with oculocutaneous albinism or OCA, while others may appear to have dark hair with albinism in their eyes only and be diagnosed with ocular albinism or OA.
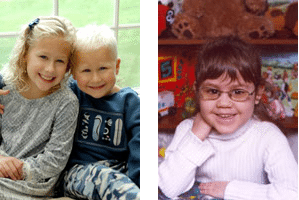
All of these children have Hermansky-Pudlak Syndrome
The visual impairment in people with HPS is the same as the visual impairment in other types of albinism. It is a result of abnormal development of the retina and optic nerves. This causes decreased visual acuity which is frequently severe enough to be considered legal blindness. People with HPS, like those with others types of albinism, also experience photophobia (light sensitivity), strabismus (crossed eyes), and nystagmus (involuntary movement of the eyes). Visual acuity typically ranges from 20/50 to 20/400. All people with HPS have nystagmus. Often the nystagmus can become more obvious when a person with HPS is tired, anxious, angry or under stress. This nystagmus may lessen with age. People with significant pigmentation (brown hair, brown eyes) may not know they have albinism. Nystagmus may be the only outward indicator of HPS.
See standard of care
Use of aspirin, ibuprofen and drugs (both prescription and over the counter) that affect platelet function can make the bleeding tendency worse! Ask your doctor and your pharmacist before taking medications. List of drugs to avoid.
Hermansky-Pudlak Syndrome involves a bleeding disorder caused by a platelet defect.
Platelets are involved in one of the mechanisms that exist within the body to counteract bleeding. Platelets are made in the bone marrow and circulate in the bloodstream in large quantities. They act directly to plug small leaks in vessels by clumping (aggregating) and obstructing flow, and indirectly by releasing substances that trigger a chain of events that culminates in a clot.
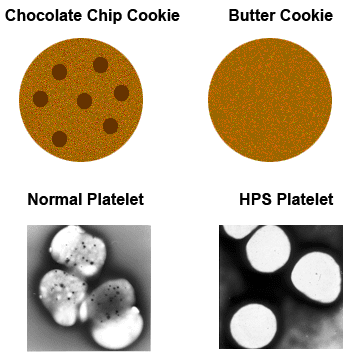
These chemical substances: ADP, serotonin, calcium, ATP, phosphate, are normally stored in platelet dense granules. These dense granules are little sacs, or compartments, that are embedded in the outside membrane of the platelet. Filled with the stored chemicals they look like “chips” and the platelets appear to look like a “chocolate chip cookie” under an electron microscope. These chemical substances are destined to be released to assist in clotting. In Hermansky-Pudlak Syndrome, these dense granules are missing; therefore, no substances are released. The platelets appear to look like a “butter cookie” instead of a “chocolate chip cookie” under an electron microscope.
Standard laboratory blood test results are not abnormal in HPS. Prothrombin time (PT), partial thromboplastin time (PTT), and platelet counts are all normal in HPS. Bleeding times can be normal though they are often prolonged. The clinical result of the defect in HPS can be seen in a bleeding tendency that varies from quite mild and hardly noticeable to life threatening. There is a possibility that people with HPS that encounter severe bleeding problems might also have a decrease in platelet von Willebrand’s factor activity, another blood component responsible for normal clotting.
Viewing prepared platelets under the electron microscope is a definitive diagnostic test for HPS at this time; however, commercial genetic testing is available in limited cases. Since all the genetic variants of HPS have not been identified, diagnosis through gene testing is not necessarily comprehensive. Once HPS is confirmed it might be helpful to gene test to know your HPS type. This could give you more information regarding future symptoms. If you need help with any diagnostic efforts please call us at 1(800) 789-9477. For more detailed information click here.
Symptoms of platelet dysfunction
People with HPS may have a tendency to bruise easily. They may experience frequent nosebleeds or when cut, tend to bleed longer. Some people with HPS may have unusual bleeding episodes such as heavy menstrual bleeding and/or bleeding with dental procedures. The bleeding problem of HPS is variable and may be mild. In some situations this platelet defect may cause life threatening bleeding, (e.g. surgeries, gastrointestinal bleeds, trauma, platelet altering medications). When treated with appropriate interventions, this serious bleeding could be prevented or resolved. Since this platelet defect cannot be identified in an emergency room or during preoperative screening, it is imperative that diagnosis is confirmed to prevent serious complications.
NOTE: Depending on your HPS gene type it is important to prevent the development of antibodies from platelet transfusions.
See standard of care
When the intestines become affected it can cause a problem that resembles a common disease called Crohn’s disease. Upon colonoscopy (a procedure done using a scope to visualize the inside of the colon) granulomas or sores, may be seen skipped around the intestines. Also similar to Crohn’s disease, inflammation and ulcerations can occur through membranes and fistulas, fissures and rectal tags may occur.
The typical age of onset for HPS Inflammatory Bowel Disease (IBD) is similar to the age of onset for Crohn’s, the teen years. Only 15 percent of people with HPS develop IBD.
Management of the IBD of HPS can be challenging. In some cases the question arises whether the problem is bad bleeding, or bad bowel disease? Careful discussion should take place between you and your doctor before considering surgical options.
Symptoms of inflammatory bowel disease
The IBD of HPS may cause diarrhea, weight loss, cramps, and blood in the stool. Some individuals report experiencing joint pain, mouth sores and in a few cases, Pyoderma Gangrenosum (a chronic noninfectious condition that causes skin ulcers).
NOTE: Individuals diagnosed with the IBD of HPS might possibly risk needing transfusions of platelets and/or blood, sometime in the course of their disease. These transfusions can potentially cause antibody production and might be a concern with some gene types of HPS.
See standard of care
In HPS type 1, 2 and 4 pulmonary fibrosis is a common problem. Pulmonary fibrosis is a scarring of the lungs which prevents them from being able to expand and contract during inhalation and exhalation. It is a restrictive lung disease. In HPS, the typical age of onset of symptoms occurs in a person’s mid-30s (although some cases occur in individuals in their early 20s). Without treatment death typically occurs between age 45 and 55. Treatments are being investigated at the National Institutes of Health. Lung transplantation is an option for some. The HPS Network is also working closely with researchers investigating gene therapy and other scientific advancements to better understand and treat HPS. Please consider participating in research and donating to our research efforts.
Symptoms of pulmonary fibrosis
When lungs become affected, shortness of breath, exercise intolerance, and abnormal fatigue might be a sign. Often patients report being diagnosed with asthma. As symptoms progress, people with HPS may have a chronic dry cough.
See standard of care
HPS is an autosomal recessive disorder, meaning it is expected to be carried by both parents. When two people carrying an HPS gene have a baby, they have a 25 percent chance, with each pregnancy, of having a child with HPS. They have a 50 percent chance, with each pregnancy, of having a child that carries an HPS gene, but is unaffected. Finally, there is a 25 percent chance that the child will not have HPS or be a carrier.

- HPS Around the World
HPS occurs in all nationalities around the world.
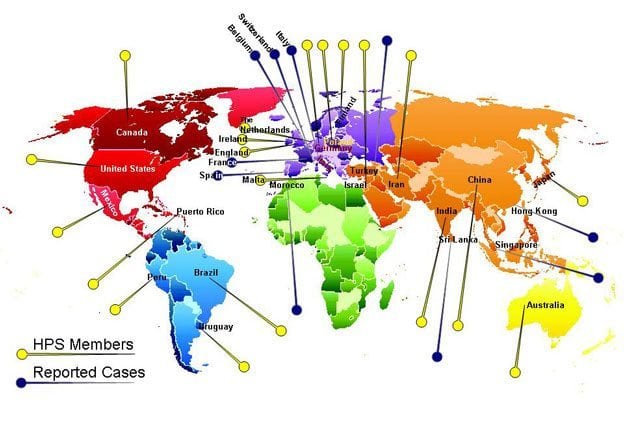
HPS1 is extremely prevalent in Puerto Rico. One in 20 people in the northwestern part of Puerto Rico carry the HPS1 gene. One in 1,800 in this region have HPS1. HPS3 is also common on the island, primarily in the central region. One in 60 people on the island are carriers of the syndrome.
However, across the globe, the incidence of HPS is 1-9 per 1,000,000. (geneReviews – NCBI Bookshelf) This is a conservative estimate because the disorder is so frequently undiagnosed.
Researchers believe HPS may also occur with greater frequency in Japan and Switzerland. Obviously, the incidence is markedly higher in the albinism community but more research is needed.

